What are the diseases of the cornea?
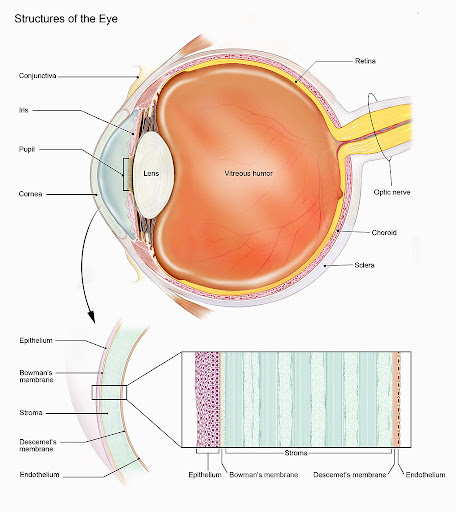
The cornea is the clear and dome-shaped layer within the eye that protects the iris and lens, helping to focus light on the retina. Made up of fluid, cells and protein, the corner serves as a barrier for the eye against dirt, germs and other harmful particles while filtering out some amount of the sun’s UV rays.
Corneal diseases pertain to a range of conditions that affect the cornea of the eye such as hereditary disorders, degenerations or infections. Corneal diseases can bring about:
- Blurred vision
- Tearing
- Pain
- Redness and inflammation
- Scarring
- Extreme sensitivity to bright light
- Headache, nausea and fatigue
Ocular herpes (herpes of the eye)
Ocular herpes is caused by the herpes simplex virus I (HSV I) and it is a viral infection that can be reoccurring. A person with the disease will have sores on the surface of the cornea which can lead to reduced vision and scarring.
Though there is no cure for ocular herpes, it can be controlled with antiviral drugs. HSVI is the same virus that causes cold sores.
Keratitis
Minor injury, bacteria, fungi, viruses or parasites can cause inflammation on the cornea. In neurotrophic keratitis, there may be a loss of sensation in the cornea with progressive damage to the top layer of the cornea that includes ulceration, thinning and even perforation in more severe cases.
Herpes zoster (Shingles)
Shingles occurs among patients who have previously experienced chickenpox. The chickenpox virus is usually inactive within the nerves of the body, but a reoccurrence can affect various parts of the body such as the eye. The affected nerve fibres can cause blisters or lesions on the cornea, fever and pain.
Antiviral treatment may be prescribed to shorten the effect of the disease but some patients may develop chronic inflammation, leading to the need for long-term eye drops or corneal surgery. There is an increased risk of shingles among older adults and people with weakened immune systems.
Dystrophy
In addition to the above, there are over 20 diseases that cause structural problems with the cornea – known as corneal dystrophies
-
Keratoconus – A progressive condition that affects the cornea structure, making it thinner, presenting a bulge and forming an irregular conical shape.
-
Fuch’s dystrophy
-
Map-dot-fingerprint dystrophy – Abnormal folds and reduplicants of the epithelium, commonly affecting patients above the age of 40. Epithelial erosions (corneal abrasions) may occur, exposing nerves that line the cornea and cause pain. The curvature of the cornea may change, leading to astigmatism and nearsightedness.
-
Lattice dystrophy – Presence of abnormal protein fibres in the stroma, possibly happening during childhood. Clear overlapping lines of protein in the stroma can make the cornea cloudy and reduce vision.
Treatment for diseases of the cornea
While some conditions can be treated with prescription eye drops and pills, more advanced diseases may require:
- Corneal transplant surgery – Performed when the cornea cannot be repaired. The eye surgeon may remove the damaged part of the cornea and replace it with healthy corneal tissue obtained from a donor. A lamella keratoplasty (partial thickness transplant) may be performed where only diseased tissue is removed, leaving healthy corneal tissue in place to maintain better structure and reduce the risk of complications.
- Laser treatment – Phototherapeutic keratectomy (PTK) is a form of laser that may be used to reshape the cornea and remove scar tissue so that you may have clearer vision
- Artificial cornea – Ophthalmologists may recommend replacing a damaged cornea with an artificial alternative, called a keratoprosthesis (KPro). It is also suggested when corneal transplants are unsuitable or do not yield satisfactory results.
Diagnosis
Only trained eye doctors can properly diagnose eye conditions. Our specialists at Eyecentric BTMC are always ready to take you through a comprehensive eye exam to ensure you have the best chances of maintaining your sight.
Prevention of corneal diseases
Avoid bacterial infection and virus by protecting your eye from injury and limiting physical contact with people who have conjunctivitis. Avoid sharing contact lens solutions, lens cases, eye drops, eye makeup. Be sure to wash your hands thoroughly regularly, especially after contact with an infected person.